As I said in earlier posts, HIV arrived in Kenya and remained unnoticed until the 1980s. It is said to have spread rapidly throughout the 80s, especially in certain places (such as Nairobi, Mombasa, Nyanza province and perhaps a few others), but also to have remained low in other places (such as the North and Northeast). The rate of new infections, incidence, peaked in the early to mid 1990s and declined thereafter. So prevalence peaked in the late 90s or early 2000s, with high death rates, which may have peaked in the mid 2000s. The epidemic has a long early years tail (1950s-1980s), a humped back, possibly very humped, and a longish neck. Perhaps the curve resembles an outline of a diplodocus, complete with a little bump where the head should be, but just a small head.
With prevalence peaking at a little over 10%, but only for two or three years, the period of high transmission or incidence would have been six or seven years previously (going backwards again, for a moment). That suggests something catastrophic in the mid to late 1980s and early 1990s that was responsible for much of this rapid transmission. Whatever that something was, it didn't result in rapid spread of HIV before the 1980s, and it ceased in the 1990s. It also ceased to result in rapid spread of HIV after a brief few years. Does that sound like sexual behavior to you? It does to the HIV industry, who have been trying to redescribe similar phenomena in all high HIV prevalence African countries.
So the diplodocus is not the only kind of epidemic curve; there are several dinosaur-like curves that you can spot using UNAIDS data. Many of them look very similar, but there are some whose backs rise two or three times higher than any of those found in East Africa, for example Zimbabwe. A few more countries show an epidemic that exploded in the 1990s but haven't dropped yet, such as Swaziland and Lesotho. The Dinosaur is also a good metaphor for some of the institutions and international NGOs that have systematically resisted one of the best arguments for universal primary healthcare ever (HIV, that is), and continue to resist it to this day. HIV is almost all a matter of individual sexual behavior, they say.
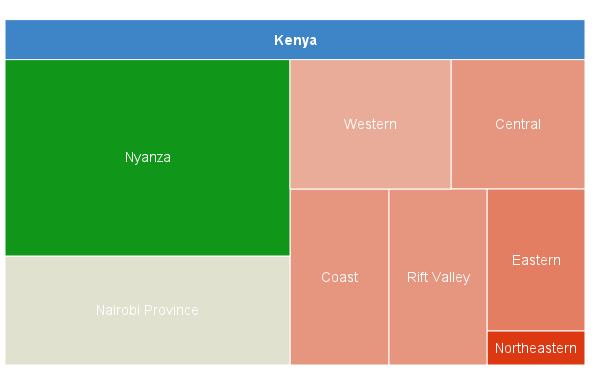
But I did mention being drawn to spatial and temporal factors, rather than 'populations'. Even in my first attempt at characterizing Kenya's epidemic it was clear that there wasn't really a 'national' epidemic. Instead, there were places where HIV prevalence was exceptionally high, and even more places where HIV prevalence was low. Over time, there were places, high and low prevalence, where the curves looked nothing like dinosaurs. They were more like pancakes in low prevalence areas, sometimes with a small piece of fruit under them, and Mexican hats in high prevalence areas. Could this data really describe sexual behavior over time? I was skeptical, not believing that almost all HIV could be sexually transmitted, as the HIV industry was claiming.
Then it was confirmed to me that HIV is frequently transmitted through unsafe healthcare, cosmetic and traditional practices, such as reused syringes and other equipment and practices in all three scenarios, with the second and third involving razors and other sharp objects that are used to pierce the skin, often the same ones over and over again, without any attempt at sterilization. Reasonable people were arguing that various kinds of bloodborne transmission were the only phenomena that could explain the Mexican hats. That accorded well with what I could glean from the literature. It just doesn't accord with what the HIV industry insists: we know it's all about sex, they insist, even when you present instances where it couldn't possibly be.
I can give you about 50 reasons why I don't believe HIV is entirely a matter of sexual behavior without even putting much thought into it (I've already written the list). But here are 10, with supporting links, so you can follow them up if you are interested. I'll supply more in Part VI, perhaps even the rest, I'm not sure yet. Many of the reasons I give overlap with the factors involved in HIV transmission that I listed in Part IV, so if you wondered about any of them, you'll probably be able to match the two lists, eventually. I may even merge them some time, but not now.
1 Prevalence is often higher among rich people. Consult the Demographic and Health Survey (DHS) for most African countries with serious HIV epidemics and you’ll find this. There is a table of HIV prevalence by wealth quintile that I drew up and it is available on a linked blog post I wrote recently.
2 Prevalence is often higher among better educated people. Again, the DHS gives data on this for all high HIV prevalence countries, but here's a graph with some of the data in a table.
3 High prevalence often clusters around transport infrastructure. Here's a wonderful map of Africa where you can see why there are the several HIV regions I mentioned in an earlier part. But notice that 'spatial accessibility' or 'friction' that they mention do not explain all the regions. West Africa has a less serious epidemic than both East and southern Africa, yet there is good transport infrastructure there.
4 High prevalence often clusters around big employers, such as mines, plantations, etc. But miners and those employed in large numbers face other threats, such as employer supplied healthcare, public health programs, tests, checkups, STI programs and whatever else. Some may face additional sexual risks when they spend 11 months of the year in an all male hostel, but anyone who thinks that this sub-human treatment only impacts on victims' sexual behavior needs psychiatric assessment.
5 Prevalence is usually higher in urban areas (where non-sexual risks are also higher). But there are multiple differences between urban and rural areas, only some of which relate to sexual behavior. The HIV industry loves going on about 'sexual networks', and not just in African countries. But what about the appalling conditions most urban dwelling people experience when they are born in a city or when they move to one? Slums are dangerous places, where children die of water borne diseases that cost a few cents to cure because what they need is clean water, to ensure they don't get any of a multitude of waterborne diseases. Babies and children die of pneumonia and various respiratory problems, again, easily avoided and treated. But even if you pump a child full of available vaccines and send them back to the same environment, many of them will just die of something else. Adults die of all kinds of things as well, often as a result of the terrible living conditions. Many die or are disabled by road traffic accidents and other kinds of serious injury. Slums, where about 75-80% of Kenya's urban dwellers live, are dangerous. Does anyone who has thought about it really think the only risks they face are sexual?
6 Prevalence is usually lower in rural areas (where non-sexual risks are also lower; have a look at any DHS). This is not to say that people don't face hazards. They also don't receive the benefits of public health programs that are available to people in the cities. Of course, this can protect them from healthcare associated HIV and other diseases but many vaccines work well, a lot of common diseases can be prevented or cured. However, when it comes to HIV, rural dwellers seem to be a lot better off, and inaccessibility of healthcare facilities may have protected them, at least in the recent past. My guess is that while some may be involved in 'sexual networks', just as people all over the world are, these do not explain everything.
7 HIV prevalence is not particularly closely related to ‘unsafe’ sexual behavior. For example, DHS figures for sexual behavior among young people in Zimbabwe show how tenuous the connection is. Even the authors were unable to interpret them. But a careful look at sexual behavior figures for many countries show that the numbers engaging in these behaviors tend to be a lot smaller than the numbers not engaging in them. These levels of 'unsafe' sexual behavior would not be able to explain the Mexican hat graphs in Nyanza and in Kenya's major cities.
8 Prevalence is often lower among those who never use condoms. As the linked article shows, condom use is often associated with higher rates of transmission than non use. The authors try to imagine arguments to show why condoms look like they are failing more often than not, but they don't come up with anything convincing. The figures in the article have been superseded and there's a more up to date table in a blog a wrote a short time ago. My guess is that condom use is higher among urban dwelling, better educated, wealthier, employed people, and that's why you get these same patterns for condom use in so many countries. Again, this strongly suggests that HIV is not purely a matter of sexual behavior.
9 HIV prevalence is low in areas where ‘intergenerational’ marriage and sex, that is, between people of very different ages, are more common. I'm linking to a blog post I wrote recently, no point in repeating the whole thing again. The data is from DHS for various countries.
10 HIV prevalence is low in areas where ‘traditional’ practices are more common, such as traditional medicine. These tend to be more common in rural and isolated areas. A possible exception to this is genital mutilation. There are two kinds, only one of which is 'traditional'. The first kind takes place in a health facility, so that's usually male genital mutilation. The second kind does not take place in a health facility and includes male and female genital mutilation. It's hard to say which is more likely to transmit HIV. If mass male circumcision was being carried out in a health facility where infection control procedures were not followed properly, not an uncommon occurrence, then healthcare associated transmission could be very likely, and would be serious; some practitioners are carrying out twenty operations a day, apparently. Traditional circumcision, which has its own hazards, is carried out in entirely unsterile conditions and adverse events are common. But it may be less likely that a HIV positive person is being circumcised along with other initiates. Prevalence should be low among young uncircumcised males. Even if they engage in sex before the wound has healed, those with whom they have sex should also be less likely to be infected. But whether done in a clinic or in a field, genital mutilation is risky. Female genital mutilation generally takes place in unsterile conditions and the risks of some forms may be higher than those faced by males. But female genital mutilation is also more likely to take place in rural areas, where HIV prevalence is lower. It is said that almost 100% of Ethnic Somalis in Kenya's Northeastern province, both male and female, are genitally mutilated, but HIV prevalence is very low.
HIV probably did very little for years in Kenya. But next to nothing for years is the way to go from being a species jump that should never have survived to being a pandemic. Perhaps a clearer history of how it survived and spread, to explode in the late 80s or early 90s, will tell us more about what is still driving transmission, in Kenya and elsewhere. But there are already many reasons for believing that HIV is not only transmitted through sex. One would want to be seriously disturbed to interpret every factor involved as evidence of sexual behavior.